How To Clean A Diabetic Foot Ulcer
Introduction [edit | edit source]
Complications in the diabetic foot are mostly caused past a triad of ischemia, diabetic neuropathy, and infection. [one]
Statistics about the impact of diabetic human foot complications:[one]
- Foot ulcer complications are the main reason why people with diabetes are hospitalized and accept to undergo amputations.
- 20-40% of all the health intendance costs comprised for diabetes are for diabetic foot complications
- 7-10% of patients with diabetes and neuropathy will develop an ulcer; this increases upwards to thirty% for patients with diabetes and other comorbidities.
- 5-8% of patients volition undergo a major amputation 1 year afterwards developing a diabetic ulcer.
- A foot ulcer preceded 85% of diabetes related amputations.
- "Diabetes increases the risk of amputation viii-fold in patients aged >45 years,viii 12-fold in patients aged>65 years and 23-fold in those aged 65––74 years."
More information on Diabetes is bachelor from these Physiopedia pages: DM Type ii and DM Type 1, Diabetes
Specific Pes Conditions [edit | edit source]
Diabetic Neuropathy [edit | edit source]
Due to diabetic neuropathy patients practice not have the protective sensation in their anxiety. Thus the patient volition not feel whatsoever trauma, like stepping

on something sharp or wearing tight shoes. This could pb to continuous tissue damage, ulceration, foot deformities, increased plantar pressure, and infection. [2]
Diabetic Neuropathy
Diabetic Foot Ulcers and Delayed Wound Healing [edit | edit source]
- In the diabetic pes peripheral arterial disease (PAD) is seen as the primary crusade for vascular impairment.[1]

- The take a chance of developing PAD is increased with diabetes and ischemia is considered the biggest culprit delaying wound healing.[ane]
- Diabetic neuropathy and ischemia combined is called neuroischemia. In these cases the wound healing is affected past the severity of the ischemia.[1]
- Diabetes Mellitus and Diabetic Ulcers
Diabetic Human foot Infections [edit | edit source]
- The well-nigh common sign is increased ulcer exudation rate.[one]
- Diabetic foot infections may lead to poor glycemic control. [1]
- At that place is a 50% delay in diagnosing deep foot infections in diabetes patients because the infection markers in their claret tests are found absent-minded. [one]
- Infections in a diabetic foot can quickly spread to the balance of the body and if not treated properly could atomic number 82 to a life-threatening full general septic infection [1]
Charcot human foot/articulation [edit | edit source]
Charcot foot also known as Diabetic foot arthropathy is a complication of diabetes and can lead to amputation if left unmanaged. It affects the joints and bone structure of people with neuropathy. Although it is more than common in diabetes to affect the foot information technology tin also bee seen in the genu, hip and spine.[3]

Symptoms may be business relationship and present and can include[iii]:
- inflammation
- redness
- warm to bear upon
- dislocation, caused past instability of the joints
- musculus weakness in the feet, ankles, legs and hands
- bony protusions on the plantar aspect of the human foot
- an awkward way of walking (gait)
- deformation of the foot
- numbness in the feet, artillery and hands
Assessment [edit | edit source]
Clinical Examination according to Lep¨antalo et al. [1]
- History
- General (Medications, diseases, cardiovascular adventure factors, work, hobbies, lifestyle, diabetes symptoms/complications
- Foot specific (risk factors and information nigh nowadays ulcer – duration, treatment, aetiology)
- Inspection (at to the lowest degree once a yr)
- Vascular
- Dorsalid Pedis Pulse
- Tibialis posterior pulse

- Venous refilling time - >5sec on dependency
- Foot appearance
- Neurological
- x-gram (5.07) Semmes––Weinstein monofilament
- Vibration(128 Hz-tuning fork)

- Pinprick discrimination and tactile sensation on the dorsum of the foot
- Achilles tendon reflexes
- Observe for foot deformities or bony prominences
- Ulcer – expect for perfusion, extent and size, and infection
- Infection
- Local signs and symptoms of inflammation: purulent secretion, redness, warmth, swelling, pain, delayed healing, and or bad odour.
- Systemic signs: fever, and poor general status
- Increased exudation in the ulcer
- Ten-rays to determine the presence of strange bodies, gas, osteomyelitis, osteolysis, or joint effusion
- MRI, os scan or CT scan to make up one's mind the extent of the infection
- Non-invasive vascular studies
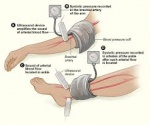
- Ankle pressure level
- Ankle-brachial systolic pressure index (ABI) (<0.6indicates significant ischemia in respect to wound healing)
- Toe pressures (<30 mmHg indicates severely impaired healing)
- Vascular imaging
- Sub-talar ROM (any reduction may increase plantar pressures during walking) [2]
Diabetic foot/stump cess form
[four]
Management / Interventions [edit | edit source]
Concrete Therapy [edit | edit source]
- Concrete Therapists are involved in both the prevention and management of diabetic foot complications. [five] This is done by gait, posture, and pes off-loading pedagogy and preparation.[5]
- Diabetes Medical and Physical Therapy Direction
- Ankle and human foot arthropathies Medical Management
- Physical Action in Diabetes
- Diabetic foot Management
- Diabetic Neuropathy Management/Intervention
- The Physical Therapist is as well involved in the rehabilitation process afterwards an amputation.
Patient didactics [edit | edit source]
Diabetic Foot Care [edit | edit source]
- Inspect your feet daily. Bank check for cuts, blisters, redness, swelling or nail problems and inform doctor if you notice any changes.[6]
- Bathe feet in lukewarm water.
- Wash feet using a soft washcloth or sponge. Dry by blotting or patting and carefully dry between the toes.
- Moisturize your feet but not between toes every bit it can cause fungal infections.
- Cut nails advisedly. [vii]
- Never treat corns or calluses yourself.
- Vesture make clean, dry socks and change them daily.
- Article of clothing socks to bed.
- Milk shake out your shoes and experience the inside earlier wearing to bank check for whatsoever strange bodies.
- Keep your anxiety warm and dry. Consider using an antiperspirant on soles.
- Never walk barefoot.
- Keep blood sugar levels nether command.
- Exercise not smoke.
- Go periodic foot exams. [8]
- Diabetes Complication and Amputation Prevention.
- Shoes and Orthotics for Diabetics
- In a 2009 evidence-based literature review, the authors found that TENS might be effective for pain treatment in diabetic neuropathy.[9]
- The authors of a 2008 control study of 30 neuropathic diabetic patients concluded that as part of the multidisciplinary arroyo concrete therapy plays an important part in the treatment of diabetic neuropathic patients. [2]
They used the following adjunct on the treatment group every solar day for twelve weeks:- Depression level laser irradiation for x-15 minutes/session on the ulcer
- Laser biostimulation on the peroneal nerve trunk (at the fibula head) at 1000 Hz for 15 minutes
- Specific dorsiflexion and ankle ROM exercises
- Didactics on human foot care and abode exercises
Medical Management [edit | edit source]
- Diabetic Wound Care Management.
- Antibiotic treatment is indicated in all infected wounds in combination with wound care, until the infection is cleared up.[1]
- Hospitilisation, immobilisation, and IV antibiotics are indicated for limb threatening or uncontrolled infections.[1]
- Urgent surgery is indicated if the infection is "accompanied by a deep abscess, extensive bone or articulation involvement, crepitus,
substantial necrosis or gangrene, or necrotising fasciitis."[1] Lepäntaloa et al. recommend that "surgical intervention for moderate or severe infections is likely to decrease the risk of major amputation."[1]
Resources [edit | edit source]
These manufactures are recommended for further in depth reading on the bailiwick:
- Lepäntaloa M, Apelqvistc J, Setaccie C, Riccof JB, de Donatoe G, Beckerg F, Robert-Ebadig H, Caoh P, Ecksteini HH, De Rangok P, Diehml Due north. Chapter V: Diabetic Foot. European Periodical of Vascular and Endovascular Surgery. 2011;42(S2):S60-74
- Pedrosa HC, Leme LA, Novaes C, Saigg M, Sena F, Gomes EB, Coutinho A, Borges Carvalho WJ, Boulton A. The diabetic foot in South America: progress with the Brazilian Save the diabetic foot project. International Diabetes Monitor. 2004;16(4):17-23.
- Turan Y, Ertugrul BM, Lipsky BA, Bayraktar 1000. Does physical therapy and rehabilitation improve outcomes for diabetic pes ulcers?. World periodical of experimental medicine. 2015 May 20;v(2):130.
Instance Studies [edit | edit source]
- Amputation secondary to Diabetes Mellitus: Amputee Instance Study
- A 35 year sometime diabetic Ancient women, who underwent a right transtibial amputation for diabetic human foot ulcer and completed prosthetic rehabilitation: Amputee Case Report
- Diabetic patient amputation: Amputee Instance Study
- Diabetic complications leading to amputation: Amputee Instance Study
- Diabetic Patient with Bilateral Amputations : Amputee Case Study
- The Young, Diabetic Amputee: Amputee Case Written report
- Bilateral Below Human knee Amputation due to Diabetic Complications: Amputee Case Study
- Lower Limb Amputation: Diabetic Case Presentation: Amputee Case Study
- Older Diabetic Amputee with slow healing: Amputee Instance Study
Follow this link to read more instance studies.
References [edit | edit source]
- ↑ 1.00 1.01 ane.02 1.03 one.04 1.05 one.06 1.07 1.08 i.09 ane.10 1.11 i.12 1.xiii Lepäntaloa M, Apelqvistc J, Setaccie C, Riccof JB, de Donatoe G, Beckerg F, Robert-Ebadig H, Caoh P, Ecksteini HH, De Rangok P, Diehml N. Chapter V: Diabetic Foot. European Journal of Vascular and Endovascular Surgery. 2011;42(S2):S60-74.
- ↑ 2.0 2.1 two.2 Zakaria HM, Adel SM, Tantawy SA. The Role of Concrete Therapy Intervention in the Direction of Diabetic Neuropathic Foot Ulcers. Bull. Fac. Ph. Thursday. Cairo Univ. 2008 Jul;thirteen(ii).
- ↑ three.0 three.1 Dardari D. An overview of Charcot's neuroarthropathy. Periodical of Clinical & Translational Endocrinology. 2020 Dec;22.
- ↑ Youtube Video: The Diabetic Foot Test https://youtu.be/aVz-Ja9Grvg
- ↑ 5.0 5.1 Kalra S, Kalra B, Kumar Due north. Prevention and direction of diabetes: the role of the physiotherapist. Diabetes Vocalism. 2007;52 (3)
- ↑ Reiber GE. Diabetic foot care. Financial implications and exercise guidelines. Diabetes intendance. 1992 Mar 1;fifteen:29-31.
- ↑ Bakker K, Apelqvist J, Schaper NC, International Working Group on the Diabetic Foot Editorial Board. Practical guidelines on the management and prevention of the diabetic foot 2011. Diabetes/metabolism research and reviews. 2012 February;28:225-31.
- ↑ Pinzur MS, Slovenkai MP, Trepman East, Shields NN. Guidelines for diabetic foot care: recommendations endorsed by the Diabetes Committee of the American Orthopaedic Foot and Ankle Society.
- ↑ Dubinsky RM, Miyasaki J. Cess: Efficacy of transcutaneous electric nerve stimulation in the treatment of hurting in neurologic disorders (an prove-based review) Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2010 Jan 12;74(2):173-6.
Source: https://www.physio-pedia.com/The_Diabetic_Foot
Posted by: masonalfulthe.blogspot.com


0 Response to "How To Clean A Diabetic Foot Ulcer"
Post a Comment